News 12 Connecticut | CT doctors push for expanded fertility treatment for LGBTQ+ patients
As some states move to limit fertility treatments, a new bill at the state Capitol could make it easier for same-sex couples to have children.
But insurance carriers are warning that the move could raise rates for everyone else.
“HEARTBREAKING”
Dr. Spencer Richlin has helped hundreds of people get pregnant at Illume Fertility in Norwalk. But with gay and lesbian patients, as well as single people, he often has to deliver bad news.
“We have to tell them that their insurance doesn’t cover them,” he said. “And that’s heartbreaking.”
That’s because those patients don’t qualify as “infertile” under state law.
“One of our single moms-to-be – she comes in, and she’s been paying her insurance. And what she needs is donor sperm,” said Richlin. “Since she hasn’t been exposed to sperm, her insurance company – that she has been paying money for – won’t help her.”
EXPANDED COVERAGE?
On Tuesday, Richlin and other doctors urged state lawmakers to pass a bill changing the definition of “infertility” for insurance purposes.
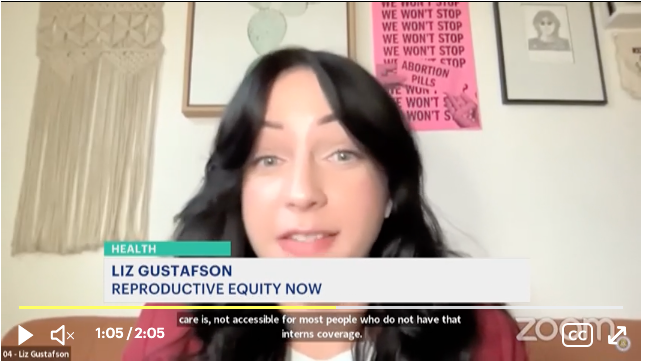
“The cost of fertility care, such as IVF, can range from $1,000 to tens of thousands of dollars,” said Liz Gustafson, Connecticut state director for Reproductive Equity Now.
The state employee health plan, which covers 250,000 people, recently expanded fertility coverage.
“Everybody in Connecticut should be able to have a child regardless of who they love, but what we know through science is that’s not possible,” state comptroller Sean Scanlon told lawmakers.
COST CONCERNS
But insurers are raising cost concerns. It’s not clear how much the change would cost, and carriers are warning it could lead to higher rates.
“And that's difficult to equate because you don't know how many people are going to take advantage of it, right?” said Sue Halpin, with the Connecticut Association of Health Plans. “You don’t know how many same-sex couples, how many single women.”
The prospect of higher premiums has small businesses worried.
“This committee should move forward with caution,” testified Wyatt Bosworth, with the Connecticut Business and Industry Association. “Mandates play a big role in the increasing costs because with each new requirement, insurers must expand coverage to include additional services or devices.”
Even if the bill passes, it would only apply to one quarter of private insurance plans – ones the state fully regulates.
DOUBLE STANDARD?
One lawmaker worries that the change would create a double standard.
“Why [do] certain individuals or couples get more protection under the law, and others don’t?” said state Rep. Cara Pavalock-D'Amato (R-Bristol).
But Richlin said it’s all about leveling the playing field.
“We can’t have people in our state feeling left out on the most beautiful thing to them, which is family-building,” he said.
The legislation may get a vote in the Legislature’s Insurance and Real Estate Committee in the next few days.